Best Hospital for Esophagal Cancer in Warangal
The esophagus is a muscular tube that connects the throat to the stomach. It is part of the digestive system and plays an important role in the process of swallowing. When we swallow food or liquids, the muscles in the esophagus contract and move the bolus (a small rounded mass of a substance, especially of chewed food) down toward the stomach.
The esophagus is about 10-13 inches (25-33 centimeters) long and is lined with moist pink tissue called mucosa. It has two muscular sphincters – the upper esophageal sphincter (UES) and the lower esophageal sphincter (LES) – which help to control the flow of food and prevent backflow of stomach acid and other contents into the esophagus.
1. Achalasia cardia
- Achalasia is equally common in both sexes
- Most commonly diagnosed between 40 and 60 years of age
- achalasia can present in any age group
History and Clinical Examination
- Dysphagia to both solids and liquids from the onset is the most common presenting feature of achalasia, as liquids require better neuromuscular co-ordination than solids for oesophageal emptying.
- Postures like raising the arms in an erect position increase the intraoesophagael pressure and propel food in the aperistaltic oesophagus, Regurgitation of undigested food (occurs in 75–91% of patients) is the second most common presenting symptom.
- Retrosternal chest pain and heartburn can be seen in 40–60% of patients, which often leads to misdiagnosis as GERD
- Weight loss can occur
- Cough and fever caused by aspiration pneumonia (8–10%) can be one of the presenting symptoms of achalasia.
Investigations
Upper GI endoscopy and timed barium oesophagogram are the initial investigations to rule out mechanical obstruction
High resolution manometry (HRM) is diagnostic and helps to classify achalasia
Upper Gastrointestinal Endoscopy
Endoscopy in achalasia shows a dilated and tortuous oesophagus and intermittent tertiary contractions
A pulsion-type oesophageal epiphrenic pseudodiverticulum can be seen
Timed Barium Oesophagogram
Timed barium oesophagogram (TBE) is the imaging of choice in achalasia
Delayed emptying of the barium from the oesophagus, tertiary contractions, and bird-beak appearance on the X-ray are the characteristic features
In late stages of achalasia, megaoesophagus (oesophageal diameter: >7 cm) and sigmoid oesophagus (dilated, tortuous oesophagus) can be seen
High-Resolution Manometry
Classifies achalasia cardia
Type I achalasia
- no oesophageal contractility or pressurization
- represents late-stage disease with a dilated, atonic oesophagus
Type II Achalasia
- characterised by panoesophagael pressurisation (in >20% swallows) between the upper and lower oesophageal sphincter
- Type II AC represents the early stage of disease
- most responsive to pneumatic dilatation (PD)
- Type II achalasia is also the most common subtype
Type III Achalasia
- least common
- least responsive to therapy
Management
In patients with low surgical risk, pneumatic dilatation, laparoscopic Heller’s myotomy (LHM), or POEM are the mainstays of treatment
Botulinum toxin (BT)/pharmacotherapy is reserved for patients with high surgical risk/limited life expectancy.
Botulinum Toxin
- The effect of therapy is short lived
- 50% of patients require reinjection after 6–12 months
- Repeat injections can be technically difficult because of fibrosis from prior injections.
Pharmacological Therapy
calcium channel blockers, nitrates, anticholinergics, phosphodiesterase inhibitors, and β agonists have been tested in achalasia
provide short-lived benefits at most
Pneumatic Dilatation
Rigiflex™ balloon dilator available in three sizes: 30, 35, and 40 mm, is used for performing PD
Initially, the 30 mm balloon is used, followed by progressively larger balloons (the graded approach)
After index dilatation by the graded approach, repeated dilatations on follow-up for recurrent symptoms is known as the ‘on demand approach’.
Peroral Endoscopic Myotomy
It is useful in treatment naïve, treatment failure, and Type III achalasia.
A contrast oesophagogram is carried out at postoperative Day 1 to exclude a possible leak and to evaluate the treatment response by seeing adequacy of barium emptying
Laparoscopic Heller’s Myotomy
LHM is the first-line surgical therapy for achalasia
a response rate of 90–97%
The minimally invasive, laparoscopic approach is associated with shorter hospital stays, reduced postoperative pain, and lower disability
2. Para esophageal Hernia/ Hiatal Hernia
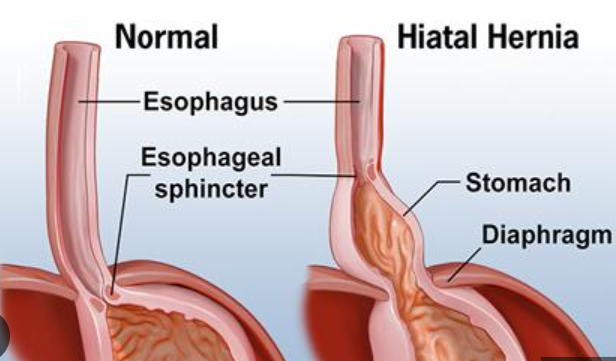
A hiatal hernia is a medical condition in which the upper part of the stomach or other internal organ bulges through an opening in the diaphragm
Classification of hiatal hernias are divided into 4 types:
- Type I (sliding type), which represents more than 95% of hiatal hernias, occurs when the GEJ is displaced upwards towards the hiatus.
- Type II is a paraesophageal hiatal hernia, which occurs when part of the stomach migrates into the mediastinum parallel to the esophagus.
- Type III is both a paraesophageal hernia and a sliding hernia, where both the GEJ and a portion of the stomach have migrated into the mediastinum.
- Type IV is when the stomach, as well as an additional organ such as the colon, small intestine, or spleen, also herniate into the chest
Etiology and epidemiology
increased prevalence in older people
typically is a result of obesity, pregnancy, chronic constipation, and chronic obstructive pulmonary disease (COPD). Trauma, age, previous surgeries, and genetics can also play a role in the development of a hiatal hernia.
History and Physical
Patients typically complain of heartburn and sometimes regurgitation. While heartburn is the most common complaint, some patients will present with extra-esophageal symptoms such as a chronic cough or asthma
Evaluation
- Endoscopy:This is an essential step in the evaluation of patients with GERD and a suspected hiatal hernia
- Manometry:
to rule out primary motility disorders such as achalasia, which can mimic the symptoms of reflux
Patients with primary motility disorders often require a partial fundoplication as opposed to a Nissen.
- pH monitoring: The 24-hour pH test is the gold standard for diagnosing acid reflux
- Esophagography: The esophagogram provides valuable information in terms of the anatomy of the esophagus and proximal stomach. Anatomic abnormalities such as tumors or strictures may also be discovered during this study.
Treatment / Management
Initial management of a patient presenting with typical symptoms of GERD in an outpatient setting includes a double dose of a proton pump inhibitor (PPI).
Patients with evidence of severe esophageal injury such as ulcer, stricture, or Barrett’s mucosa should be considered for surgical treatment
Current recommendations
operative repair of all symptomatic paraesophageal hernias as well as completely asymptomatic large hernias in patients less than 60 years old and otherwise healthy
surgical procedures
Nissen fundoplication (360-degree wrap) and Partial fundoplication (Dor and Toupet)
3. Corrosive Injury Esophagus (Acid Ingestion)
Corrosive ingestion is a common form of poisoning
Corrosive agents cause severe damage to the gastrointestinal (GI) tract. The most severe forms of injury can lead to mortality
Upper GI endoscopy is the test of choice for assessing severity in the acute phase of the disease
The long-term management is based on the site, length, number, location, and tightness of the stricture
Acidic agents, frequently responsible, are the ones that are commonly available such as cleaning agents (hydrochloric acid) and a gold solvent, which is a mixture of hydrochloric and nitric acid
Alkalis commonly used are hydroxides of sodium and potassium.
The mechanism of acidic and alkaline injury is coagulation necrosis and liquefactive necrosis, respectively
Injuries due to corrosives can be restricted to the esophagus or stomach
Coexistent esophageal and gastric injuries are seen in 20%–62.5% cases
Clinical Features
The acute phase of corrosive injuries involves perforation of the esophagus, stomach, or duodenum.
Esophageal strictures cause dysphagia.
Imaging Features
1. Plain x ray
A plain chest x ray – may demonstrate pneumomediastinum suggesting esophageal perforation
free air under the diaphragm suggesting stomach perforation
- upper GI endoscopy
- barium esophagogram
- CECT chest and abdomen
Management
Management of acute corrosive ingestion is focused on initial resuscitation, evaluation of the grade of injury, treatment of early complications, maintenance of nutrition, and prevention of stricture formation
Emergency surgery
Indication – transmural necrosis of the gastrointestinal tract
Aim- to remove all the necrotic tissue
the standard approach – laparotomy
Procedure – patients with combined esophageal and gastric injury, esophagogastrostomy with cervical esophagostomy is performed
for nutritional improvement before definitive procedure – A feeding jejunostomy
Endoscopic Management
Graded Approach – endoscopic esophageal dilatation
Surgical Management – colon pull up
Find a Specialist
Senior Surgical Oncologist
DNB – Surgical Oncology – NIMS Hyderabad, PDCC Fellowship – SVIMS Tirupathi
Consultant Surgical Oncologist
MBBS
M.S (General Surgery)
FMAS, DrNB (Surgical Oncology)
Consultant Medical Oncologist
MBBS
M.S (Otorhinolaryngology)–GMC
M.Ch (Head&Neck Surgery Oncology)AIIMS
Consultant Head & Neck Surgeon
MBBS
DNB Radiation Oncology
Consultant Radiation Oncologist
MBBS
M.D.(General Medicine)
(D.M.(Medical Gastroenterology))
Consultant Gastroenterologist
MBBS
MS, FELLOW IN HEAD & NECK SURGICAL ONCOLOGY
CONSULTANT HEAD & NECK ONCO SURGEON
MBBS
Mbbs, M.S (General And Laparoscopic Surgery)
Consultant General And Laparoscopic Surgeon